Student Research: Chronic lung disease support for premature babies
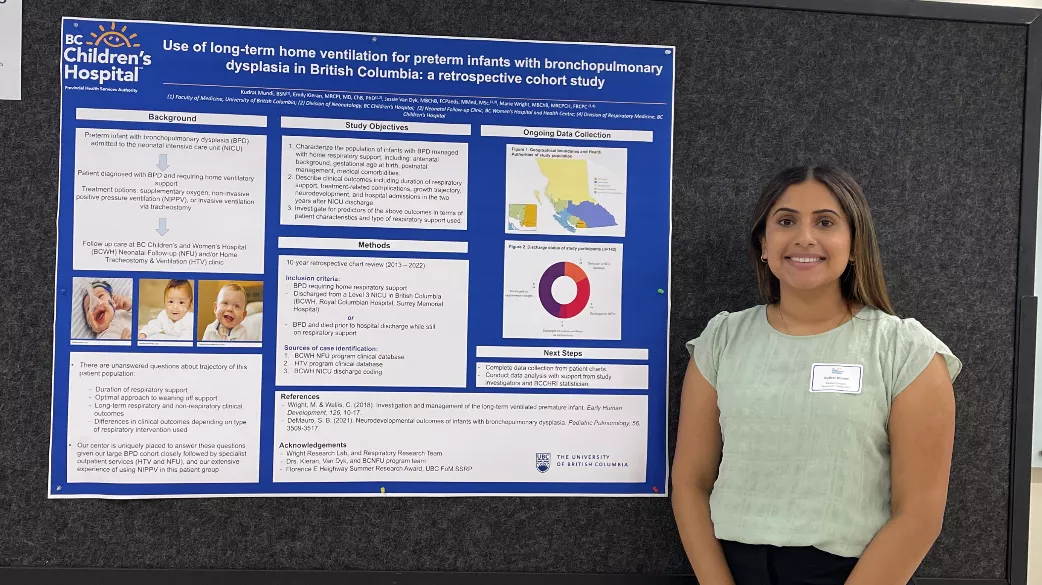
Over her summer break, NMP Class of 2026 student Kudrat Mundi undertook a pediatrics research project based at BC Children's Hospital. Her research was focused on bronchopulmonary dysplasia (BPD), a chronic lung disease in newborns related to prematurity.
What inspired you to become part of this research project?
Coming into medical school with an undergrad in nursing and knowing pediatrics was a patient population I was interested in working with, I was eager to pursue a research project based at BC Children’s Hospital. I was inspired to pursue this specific project because during my clinical experiences in nursing school, I learned that when patients are admitted to the hospital, they have a plethora of resources and services at their fingertips. However, upon discharge many of these resources and services become limited, especially for rural and Northern patients. Physicians take great consideration when deciding to discharge a patient and how to best support them afterwards to ensure optimal outcomes, and that’s what this project is working towards answering for patients diagnosed with bronchopulmonary dysplasia that require home ventilatory support.
Can you briefly explain your research?
Bronchopulmonary dysplasia (BPD), also known as chronic lung disease of prematurity, is characterized by a disruption of lung development resulting in chronic inflammation and recurrent hypoxia, in the context of preterm birth. BPD is one of the most common complications associated with preterm birth and has a significant healthcare burden. Patients with moderate to severe BPD will often require home ventilatory support upon discharge from the neonatal intensive care unit (NICU). Options for this support include supplementary oxygen via nasal prongs, non-invasive positive pressure ventilation (NIPPV), or invasive ventilation via a tracheostomy.
My project is aimed at answering questions regarding how long patients require this home ventilatory support for, optimal approaches to weaning off support, long-term respiratory and non-respiratory clinical outcomes, and how these outcomes differ depending on the time of support the patient received.
Who did you work with on this project?
My project supervisor was Dr. Marie Wright, a pediatric respirologist at BC Children’s Hospital. I also received support from Dr. Emily Kieran, Dr. Jessie Van Dyk, the BC Women’s Hospital Neonatal Follow-Up Clinic team, and the Respiratory Research Team at BC Children’s Hospital.
How did this project help further your learning as a medical student?
This project provided me the opportunity to learn about the process of starting and conducting a research project. For example, writing applications for ethics and awards, developing data collection tools, collaborating with a multidisciplinary team, troubleshooting when steps of the process took longer than expected, etc. This has been immensely helpful as it has provided me with a foundation that I can work from as I hope to incorporate conducting research into my future practice.
Doing a summer research project has been such a fantastic learning experience and I can’t recommend it highly enough to incoming medical students!