Research brings partners together to help mental health clients pursue healthier lives
Prince George, BC - A research study led by Northern Medical Program researcher Dr. Candida Graham, together with community partners, is helping to empower local mental health clients to actively pursue and maintain healthier lifestyles. With one in five Canadians experiencing a mental illness in their lifetime, health risks can be high for affected individuals if they have to face persistent illness.
“Those dealing with an enduring mental illness such as schizophrenia face the prospect of having a 20 per cent shorter lifespan due to added difficulty in dealing with illnesses such as diabetes and heart disease,” says Dr. Graham, a clinical associate professor in psychiatry with the Northern Medical Program and the Faculty of Medicine at the University of British Columbia. “Through this study, we have been working to understand how community partnerships can help positively impact client health behaviours, and overcome barriers such as stigma and the challenges associated with daily living activities when an individual is living with a mental illness.”
Partners in the study, which began in 2013 and will continue through to 2016, include the Activity Centre for Empowerment (ACE) which is operated through the BC Schizophrenia Society for the Northern Interior; YMCA of Northern BC; the Northern Sport Centre at UNBC; Chinook Yoga; Youth Around Prince George (YAP); and local health professionals.
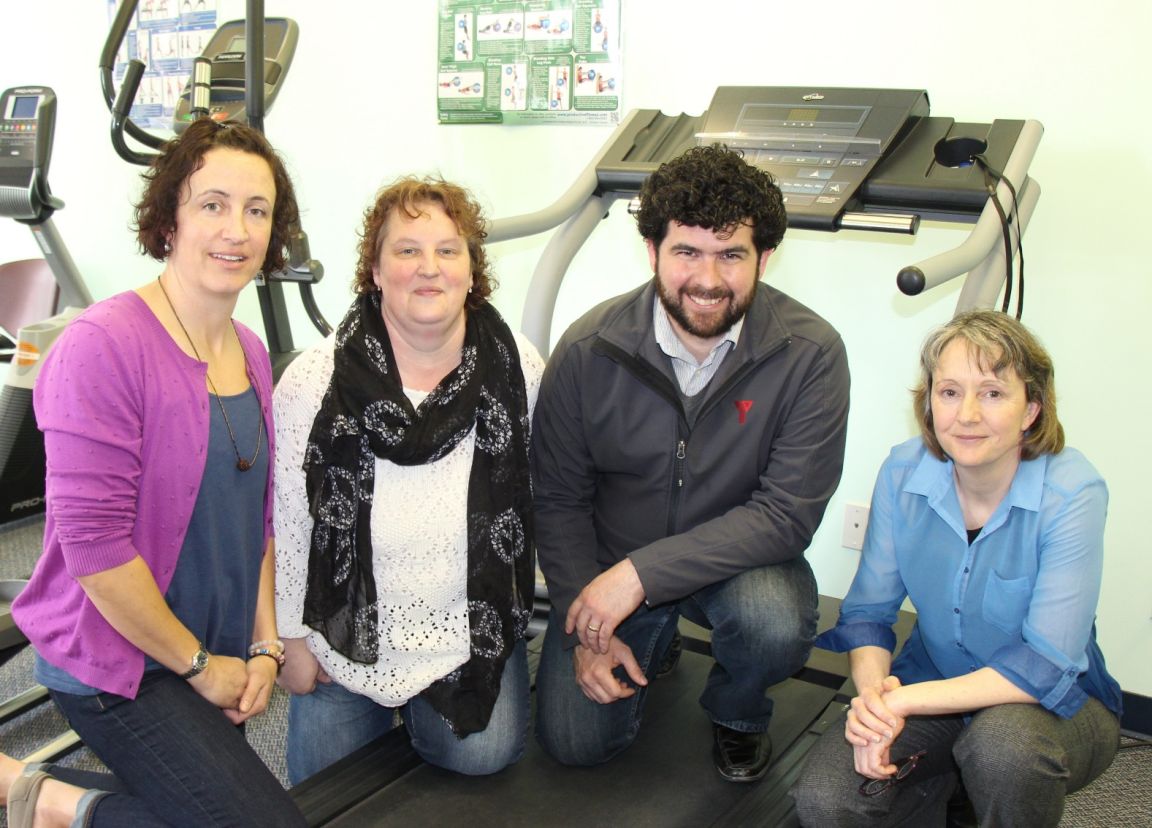
From left: Jaylene Pfeifer, Chinook Yoga; Nansi Long, Activity Centre for Empowerment (ACE); Chris Kinch, YMCA of Northern BC; and Dr. Candida Graham, Northern Medical Program. Download high-resolution version
The study has involved several community initiatives that have enabled ACE clients to participate in various health-related activities, including a walking program, yoga and fitness classes onsite at the Activity Centre, a community kitchen program, nutritional advice, a peer lead tobacco reduction program, and the sharing and dissemination of health and resource information.
“It has been really exciting to see the direct impacts of the study on the people that I am working with everyday,” said Nansi Long, a coordinator at ACE. “For example, when the delivery of our initial walking program ended in the fall of 2014, one of our clients stepped up to become a peer leader in order to enable a walking group to continue on.”
Other clients have shared their feelings of embracing and continuing their pursuit of healthy activities more regularly.
“Being accountable for my own wellness and seeing the improvements in stamina, mood, and day-to-day coping skills among my fellow participants has had a huge impact on me,” said Margaret T. “There is nothing more satisfying than knowing a shared experience has helped the whole group, each in their own ways.”
“We recognize the barriers that everyone can face in maintaining a healthy and active lifestyle, and when mental illness is involved, those barriers can become even larger,” said Chris Kinch, YMCA director of membership and programs. ”This project and ongoing partnership with ACE has made exercise more accessible to ACE clients, and provided our fitness leaders with additional tools and understanding for working with individuals at ACE and in the broader community dealing with mental health challenges.”
“We are grateful to be part of this ongoing project that allows us to bring the practice of yoga and all of its benefits to a space outside of our studio,” said Jaylene Pfeifer, owner and yoga teacher at Chinook Yoga studio. “This was and still is an opportunity that allows ACE participants access to a yoga space they are familiar and comfortable with. This is a key piece to what the participants voiced was important to them. We look forward to continuing our classes at ACE and being actively involved in this community.”
The study’s goals have included providing behaviourial lifestyle interventions that both meet client needs in overcoming barriers and empowering individuals to maintain healthy activities; and working to develop community partnerships that will continue to provide initiatives to better support client health and well-being.
The research study was funded by the Vancouver Foundation, and also received support from Northern Health and the Northern Medical Program.
-30-